What to know about being “bipolar”
Tips for getting started managing the ups and downs
Bipolar Basics
Overview
Bipolar disorders are a group of mental health diagnoses associated with mood swings. People who are identified as having bipolar disorder experience elevated mood, known in the mental health world as mania or hypomania, as well as low mood, or depression.
The Lingo
In the mental health space, these bipolar-related terms get thrown around a lot:
Mania—extreme elevation in mood, energy level, or activity level
Hypomania—literally, “below mania,” a less severe form of mania. For example, mania can involve delusions or hallucinations, while hypomania is defined as not being associated with these experiences
Manic depression—extreme forms bipolar disorder used to be called this
Depression—you probably know it when you see it. One metaphor I like: When you’re sad, your inner world is drained of color. When you’re depressed, the world around you seems to have lost its color.
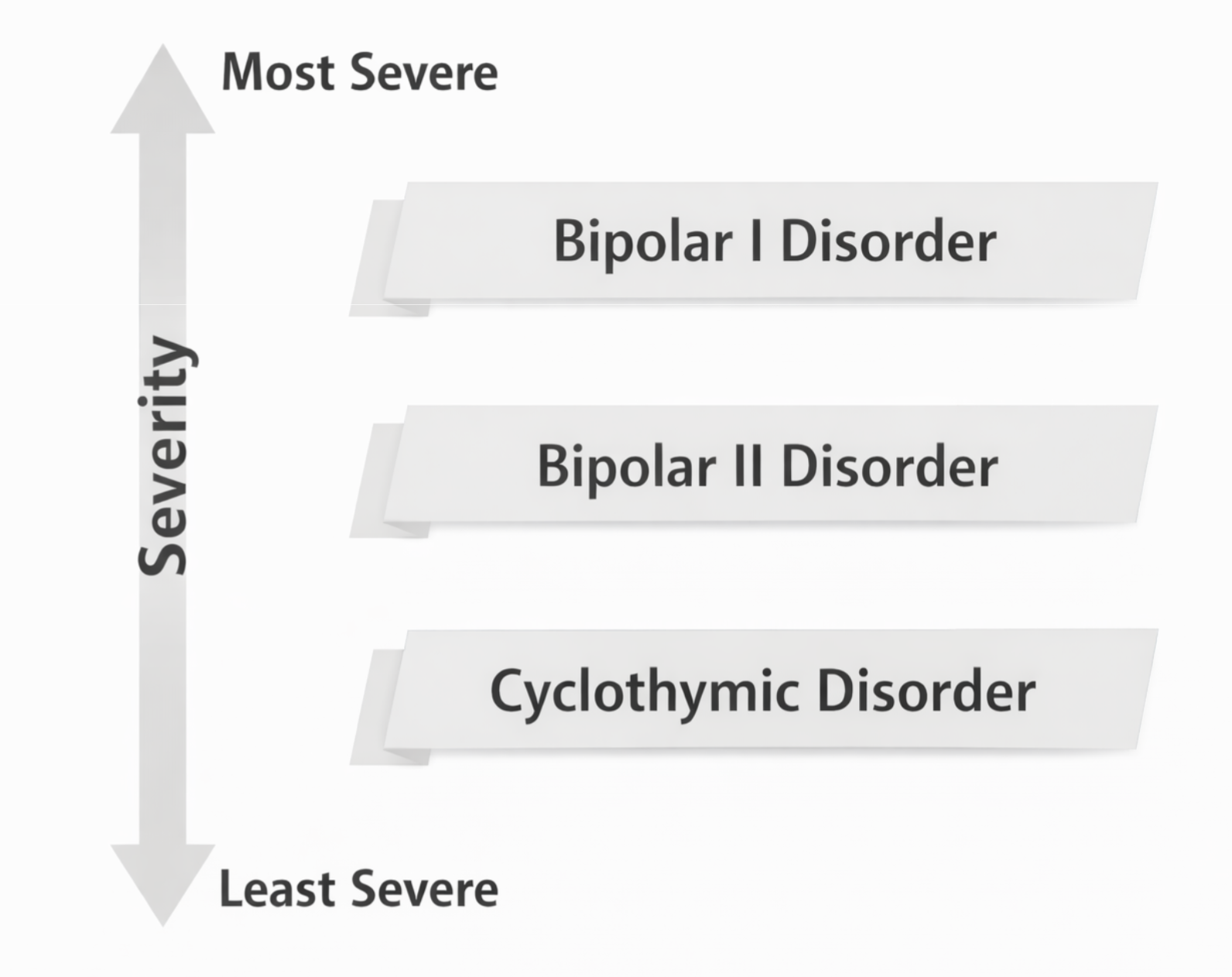
The diagnoses
Diagnoses are useful in at least two ways:
Naming things: diagnoses are shorthand for mental health clinicians to speak about clusters of symptoms that tend to happen together
Paying for things: a diagnosis is required for insurance to pay for treatment of a health condition
Here are the current diagnoses from the Diagnostic and Statistical Manual of Mental Disorders (DSM) associated with bipolar disorder:
Bipolar I—Bipolar disorder that includes an episode of mania
Bipolar II—Bipolar disorder with hypomania, but not mania; it also requires a major depressive episode to be diagnosed
Cyclothymia—Fluctuating mood that has not been significant enough to qualify for a a Bipolar I or II diagnosis
Beyond the Basics
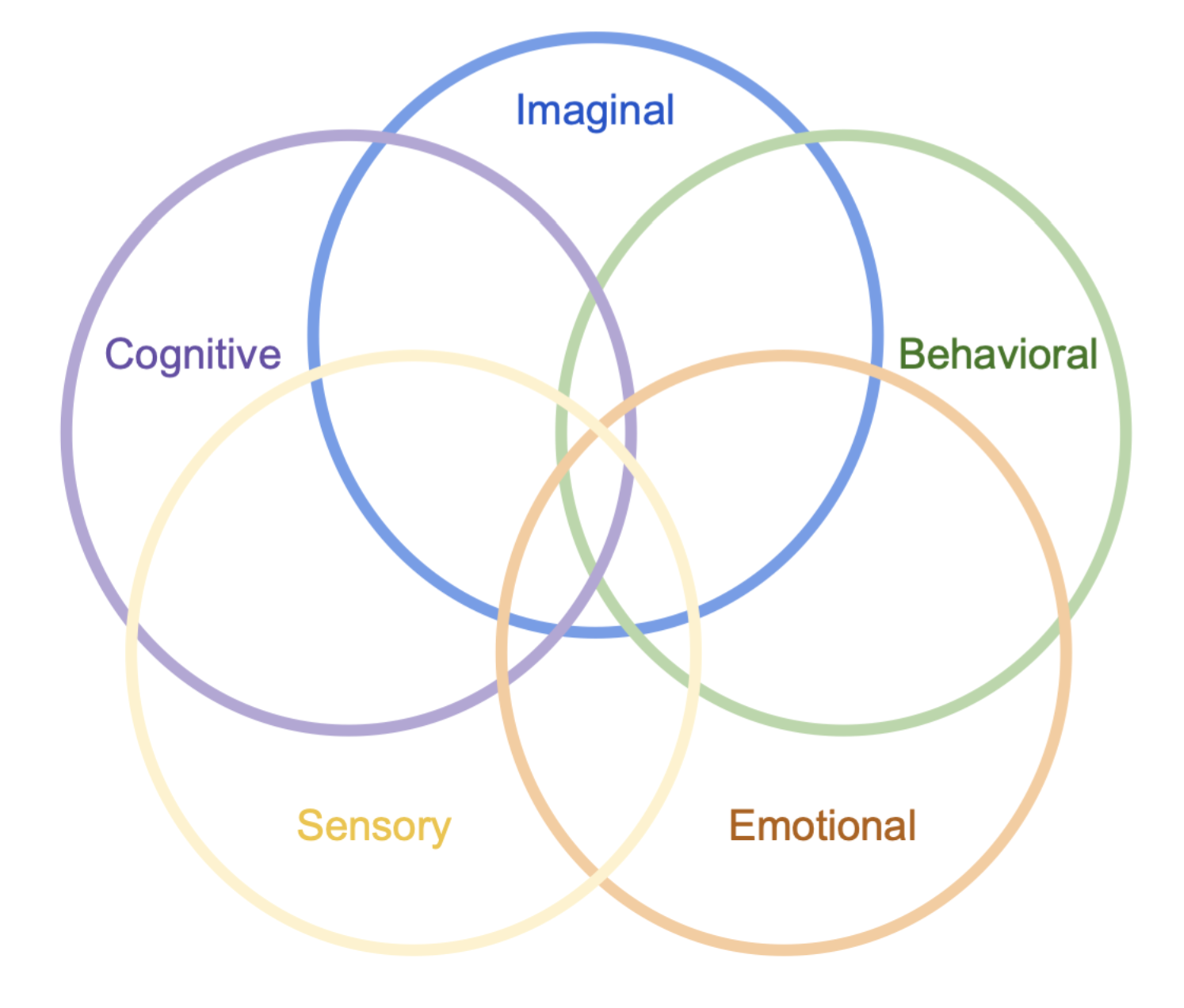
It’s not just about mood
Bipolar disorders are now synonymous with extreme mood fluctuations. Mood, however, is just one component of the experience of depression and mania. Additional dimensions of the experience of depression and mania include the:
Imaginal - this refers to a person’s inner world, the images, fantasies, and other pre-cognitive internal experience that we later try to organize into meanings, thoughts, feelings, and actions
Cognitive - thoughts are different when depressed or manic. When depressed, thoughts can be slower, fewer, and less spontaneous–mental energy is just lower. When manic or hypomanic, the opposite is true – there are more thoughts that come faster, more connections are made between thoughts, and there is often a strong confidence in the truth of one’s thoughts
Behavioral - A severely depressed person is pretty unmistakable – they can move slower and withdraw from daily activities. In mania and hypomania, there’s often increased activity, restlessness and even reduced need for rest. People in manic and hypomanic states can at times maintain their mental sharpness without sleep
Sensory - in depression, everything can feel flat or look gray, food can have less taste. In mania and hypomania, colors can be intense, things feel more alive, music can feel transcendent.
A few of the many parts of our experience…
The gifts of the ups and downs
The ancient Greeks spoke of the Muses–goddesses considered the source of literature, science, and the arts–inhabiting humans from time to time, inspiring our imagination. Contained in this mythological conception of creativity is a deep honoring of the human experience across non-ordinary states of consciousness.
While the mental health field conceives of mania and depression in terms of its risks and dangers, there can also be inspiration in experiences that are outside the norm.
Perhaps a simpler way to say that is this: your mood isn’t a problem unless it’s a problem.
What is the problem?
People with fluctuating mood often don’t report the “up” phases. They enjoy them. They feel great. They get a lot done. They can be more fun to be around. But the impulsivity that can accompany the high energy and activity can lead people to make decisions they regret later. Sleeping with people they don’t know, spending a lot of money, taking on huge projects, quitting their job, driving recklessly, using more substances than usual, or acting in ways that strain relationships.
What to do about it?
People with bipolar disorder reported that most of the effective things they did to help them were changes in daily activities. In 2013, CureTogether and 23andme published a study that suggested that, based on compiled responses from 301 people diagnosed with Bipolar Disorder, the most effective treatments are:
Regimented sleep
Reduce alcohol
Exercise
Lamictal (a medication commonly prescribed for Bipolar)
Sunlight
Yoga
Psychotherapy
Mindfulness meditation
Small, frequent snacks
Self-tracking
Regular social contact with others didn’t make the above list, but other studies suggest it can also be an essential factor in recovery from problematic mood instability.
Why are lifestyle changes so important?
Lifestyle changes are clearly a huge part of Bipolar treatment, according to folks who have it. Why? Bipolarity is associated with neurohormonal shifts. These hormones naturally shift during the day, and getting them back into a healthy rhythm is crucial to restoring stable mood. In Bipolar, Not So Much, Chris Aiken, MD, writes,
A better term [for bipolar disorder] might be “fragile circadian rhythm disorder.” That lengthy title gets closer to the root of the problem and guides you toward the best way to control it.
Regulating a fragile circadian rhythm
Studies suggest that regulating a fragile circadian rhythm starts with doing several things at regular times: going to bed, getting up, eating, exercising, and being together with other people.
With sleep ranking at the top of the list of effective treatments, some people find that being intentional about their exposure to light and darkness can be crucial to getting regular sleep, which helps with maintaining mood stability. That could mean having less exposure to artificial light in the evening, having total blackout darkness (using blackout curtains or an eye mask) when you sleep, and getting outside in the bright sunlight during the day.
Resources
Books
The book Bipolar, Not So Much–also available as an audiobook–by Chris Aiken, MD is a great place to dive into up-to-date research about bipolar patterns and treatments.
Aiken also wrote The Depression and Bipolar Workbook: 30 Ways to Lift Your Mood & Strengthen the Brain that includes techniques to work with the body in ways medication can’t.
An Unquiet Mind: A Memoir of Moods and Madness by Kay Redfield Jamison is one doctor’s story of her experience with bipolar.
Apps
The eMoods Bipolar Tracker app is available for iOS, Android, and desktop, and was developed specifically for self-tracking bipolar symptoms. This is one way to implement self-tracking.
Daylio isn’t specifically designed for bipolar disorder, but it does have options for journaling and a user-friendly interface.
Support Groups
Mountain Express keeps a list of local active support groups in Western North Carolina here. Many of the organizations listed have groups that meet in-person across North Carolina and around the world, as well as online.
Therapy for bipolar disorder
Therapy can be a good way to get support during any challenging time. With regard to bipolar disorder in particular, therapy can help with:
Mood monitoring and early intervention – identifying triggers and warning signs for mood shifts to prevent episodes from escalating and reducing their intensity
Coping strategies and accountability – therapy can provide support for putting new habits into practice to manage mood
Relationship and social support – bipolar disorder often strains relationships. Therapy can offer a space to explore interpersonal challenges and learn how to rebuild trust with family, friends, or partners
Self-understanding and acceptance – therapy can be a place to explore the intersection of mood and personal identity, life goals, and values. Getting to know oneself better can reduce shame, improve self-esteem, and
Long-term resilience – therapy can support long-term emotional regulation
How I work with patients with Bipolar Disorder
I have extensive experience working with elevated mood states. I’m familiar with the major pharmacological approaches to bipolar treatment and have experience partnering with several local medication providers in Asheville and around North Carolina.
While managing the risks associated with up mood states is extremely important when treating the challenges that come with bipolar disorder, I’ve found that working successfully with patients with fluctuating mood often requires acceptance of and appreciation for the creativity and sense of freedom and connectedness that accompany euphoria. I’ve found myself able to understand a great deal about what is deeply important to my patients by listening closely to what comes up for them when they are in elevated mood states.
When I work in therapy with folks who struggle with the more challenging aspects of mood fluctuation, I start by emphasizing behavioral approaches–those listed above as well as others that I’ve seen work for others. An early behavioral focus on mood stabilization can help patients arrive at a place where I’m able to offer a more open-ended exploration of what might be making it difficult for a person to express more of themselves when they’re in a stable mood state.
If you’d like to work with me, reach out to me here to connect for a consultation.